The following case highlights the use of the Medmont Meridia for high-definition imaging, utilising white light and blue light fluorescein capture, to monitor treatment response in anterior eye conditions.
Case presentation:
Mr. SB, a 31-year-old male, has been a long-term rigid contact lens wearer since his diagnosis of bilateral keratoconus in his early teens. He underwent corneal cross-linking in both eyes in 2009 and was subsequently fitted with scleral contact lenses in his hometown in New Zealand from 2011. He has a history of herpes simplex virus (HSV) keratitis in his right eye in 2012, followed by disciform keratitis in the same eye in 2017.
1/11/24 – Initial Consult:
Having recently moved to Melbourne, Mr. SB presented for an initial consult due to a red left eye persisting for the past two days, accompanied by significant pain, photophobia and tearing. As a result, he had not worn his left scleral lens during this period. His right eye remained unaffected, and he continued to wear a scleral lens in his right eye without issues.
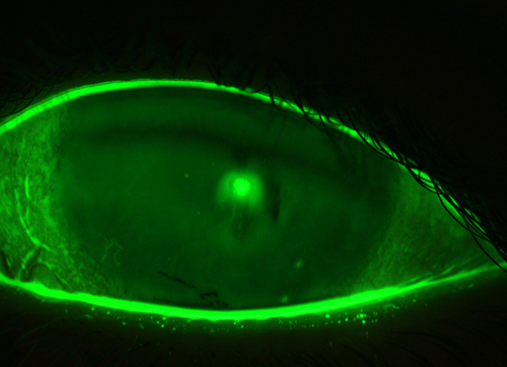
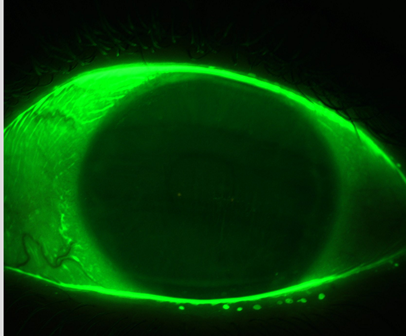
Anterior slit lamp examination revealed grade 2 bulbar hyperemia and a raised central corneal infiltrate with stromal haze and overlying fluorescein staining. The anterior chamber was deep and quiet. The Medmont Meridia was used to capture high-definition fluorescein imaging of Mr. SB’s left cornea, as shown in the image below.
As Mr. SB is a contact lens wearer and the corneal infiltrate was central and raised, he was treated conservatively as microbial keratitis (MK) in consultation with a local ophthalmologist. Treatment included Ocuflox 0.3% eye drops every two hours, with a follow-up review scheduled in three days. He was advised to refrain from wearing his left contact lens during this period.
3/11/24 Three-day review:
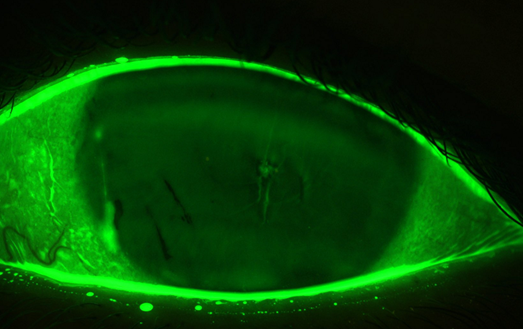
At the three-day review, Mr. SB reported significant improvement, with no redness, pain or photophobia. Slit lamp examination revealed substantial improvement; however, the corneal infiltrate remained raised with mild residual staining. The Medmont Meridia was used to document the progress.
Mr. SB was advised to continue Ocuflox 0.3% eye drops every two hours for an additional two days (completing a five-day course) and return for a follow-up review in two days.
6/11/24 – Six-day review
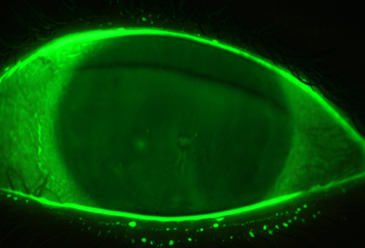
At the six-day review, Mr. SB was asymptomatic after completing a five-day course of Ocuflox 0.3%. Slit lamp examination showed significant improvement, documented with Medmont imaging. The lesion was no longer raised, with no epithelial involvement, though mild stromal haze remained. Pred Forte 1% QID was prescribed to minimize scarring.
20/11/24 – Final review
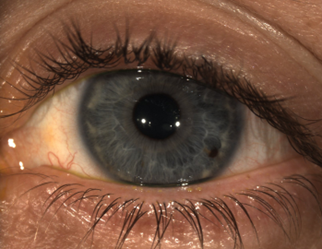
The following Medmont image documents Mr. SB’s final review, showing complete resolution of the corneal lesion. Pred Forte 1% was tapered appropriately, and he was refitted with a left scleral contact lens with increased central sag to ensure full corneal vaulting.
This report was prepared by optometrists Dr Van and Dr Rossi from Richard Lindsay & Associates.

Jacinda Van
Optometrist, Richard Lindsay & Associates

Michaela Rossi
Optometrist, Richard Lindsay & Associates
