Orthokeratologist/Optometrist Scott Brown, Clinical Director of Scotlens, highlights the importance of early detection—and why the Medmont Meridia™ should be part of your keratoconus workflow.
Topography with the Medmont Meridia™ can be invaluable in enhancing eye examinations for patients. The case outlined below highlights why topography should not just be for enhanced exams, but be considered a standard of care for patients under 30 years old. I hope to demonstrate why topography is, in my opinion, as important—if not more so—than axial length measurement in myopia management.
The reflected Placido mires provide insight into three distinct layers of the eye:
- Tear Film: Measures stability and break-up, either on the eye or on the surface of a contact lens.
- Epithelium: Shows changes, whether induced through orthokeratology or resulting from contact lens wear.
- Stroma: Can reveal structural abnormalities such as ectasia or trauma-related changes.
The corneal stroma plays a crucial role in determining the shape and power of the cornea. As the most powerful refractive component of the visual system, the cornea develops and stabilizes early in life, typically by ages three to four. Given its early stability, any measurable changes can indicate early-stage keratoconus. With the advent of corneal cross-linking, early detection significantly improves prognosis, while late detection leads to poorer visual outcomes.
Case Presentation
A 23-year-old male patient was referred to me for specialty contact lens fitting in 2020. Over the preceding two years, he experienced progressive astigmatism and changes in spectacle refraction. His optometrist updated his spectacles but did not perform topography to confirm keratoconus onset.
Unfortunately, the timing was unfavourable, as the COVID-19 pandemic delayed his access to corneal cross-linking, resulting in further progression and permanent visual acuity loss. He is now dependent on a gas-permeable contact lens for functional vision in his right eye, while his left eye requires surgery, as no contact lens could improve its acuity.
This case underscores the importance of early referral, as the delay led to a significant and preventable visual impairment.

The Role of Screening in Optometry
Screening for preventable eye diseases is a key responsibility in optometry. We routinely screen for glaucoma, even in young patients with a minimal risk, as failure to do so would be considered neglectful. Keratoconus, which develops before age 30 and has a prevalence of 1.4%, deserves similar attention. Neglecting to screen for keratoconus in young patients is akin to omitting glaucoma screening for all patients under their mid-sixties when the prevalence of glaucoma reaches the same 1.4%.
Medmont Meridia’s Role in Keratoconus Screening
The Medmont Meridia provides three essential functions for keratoconus screening:
- Colour Map: I prefer the tangential map with a standard scale, as it clearly displays asymmetries and uses a fixed scale to highlight abnormalities.
- Kmax: By switching to axial and normalized scales, the steepest corneal power is automatically detected. This single metric can be tracked over time and is more sensitive to change, particularly in decentered cones, compared to Sim Ks, which are limited to measuring the central cornea.
- Medmont Disease Indices: The traffic light color-coding is intuitive and highly sensitive to early changes, making it an effective tool for early detection.
Early Detection: A Key to Preventing Sight Loss
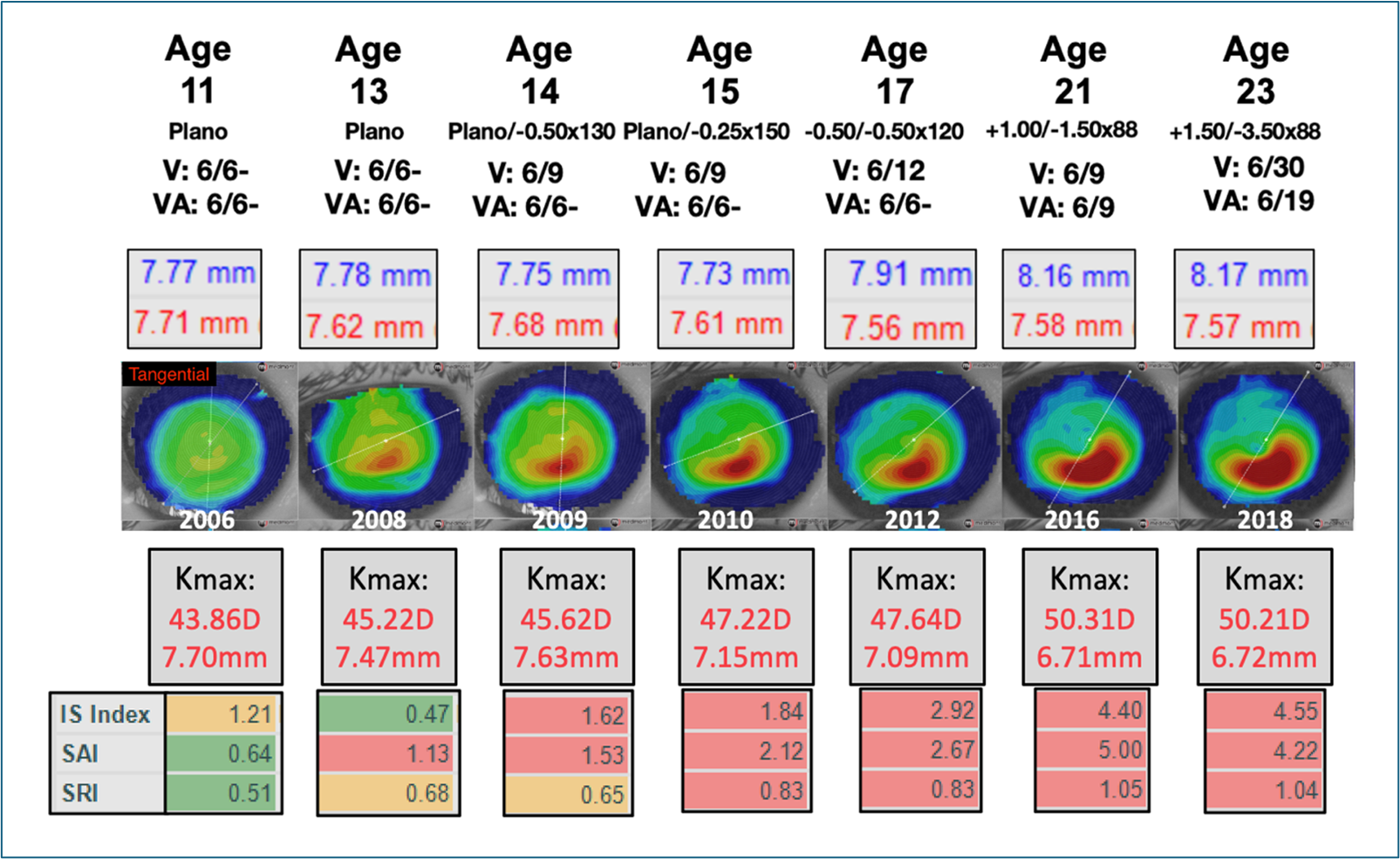
The case below shows the right eye of a patient whose left eye had a similar but slightly milder presentation. At age 17, if only refraction were considered, the patient might have been misdiagnosed with myopia. This highlights the critical importance of performing topography when any young patient presents with refractive changes. Without topography, keratoconus was not definitively identified until the patient was 21.
However, reviewing the patient’s topography retrospectively, the colour map, Kmax, and disease indices indicate keratoconus as early as age 13. These indices provide earlier detection than the traditional Amsler-Krumeich classification, which would have classified this patient as grade 1 between ages 17 and 21.
Conclusion
This case illustrates how topography screening in young patients can lead to keratoconus diagnosis years before it would be detected through refraction alone. As optometry continues to advance in myopia management, incorporating early topography screening can help eradicate sight loss due to keratoconus. I hope the profession quickly adopts this opportunity to improve patient outcomes.
