New Perspectives in Managing Dry Eye Start with Screening

Author: Aaron Wolf, O.D., Austin Optometry Group
It is undeniable that the global COVID-19 pandemic has forced the industry to evaluate its business-as-usual optometry practices and to reassess the patient experience. Most notably, there is a significant reduction in daily caseloads for the health and safety of doctors, employees, and patients.
While this means that doctors may see fewer patients in terms of quantity, they can improve each patient’s quality of care. Seeing fewer patients increases invaluable per-patient visit time and allows doctors to pivot from the “diagnose and treat” position to a “screen, evaluate, and prevent” position.
Shift the Focus from Therapeutic to Preventative Eye Care
Seeing fewer patients opens up new areas of opportunity for screening and engagement for optometry practices. As the world’s population faces increasing eye health risks with more screen time, dry eye disease (DED) is an ailment sending patients to the eye doctor more frequently. Worldwide, 352 million people suffer from moderate, severe, or episodic DED, while only 45% of U.S. dry eye sufferers have been diagnosed.
Even before the current work-from-home environment, people were spending an increasing amount of time online. And at the peak of the pandemic, screen time use reportedly spiked to 13 hours per day in the U.S. The extensive use of computers and other mobile devices decreases the frequency of eye blinks, leading to incomplete blinking, evaporation of tears, and subsequently to DED.
An emerging consequence of our current environment is mask-related dry eye. When you exhale, air is pushed over the surface of the eye, accelerating the evaporation of the tear film. As mask-wearing will likely be the norm for some time into the future and the general increase of screen time, paying attention to the signs and symptoms is extremely important. When screened adequately for and diagnosed, DED can be effectively managed, and the long-term adverse effects are later minimized.
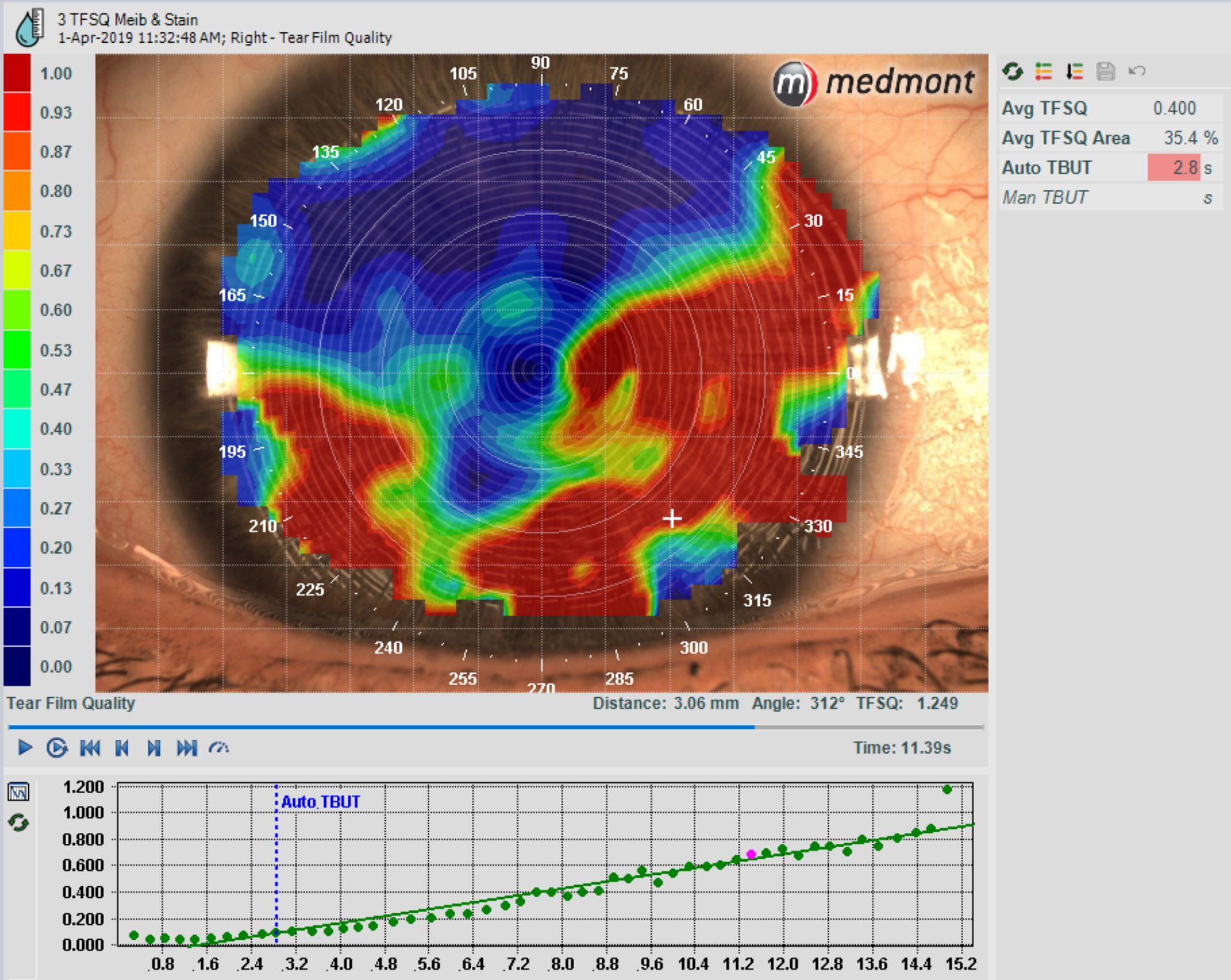
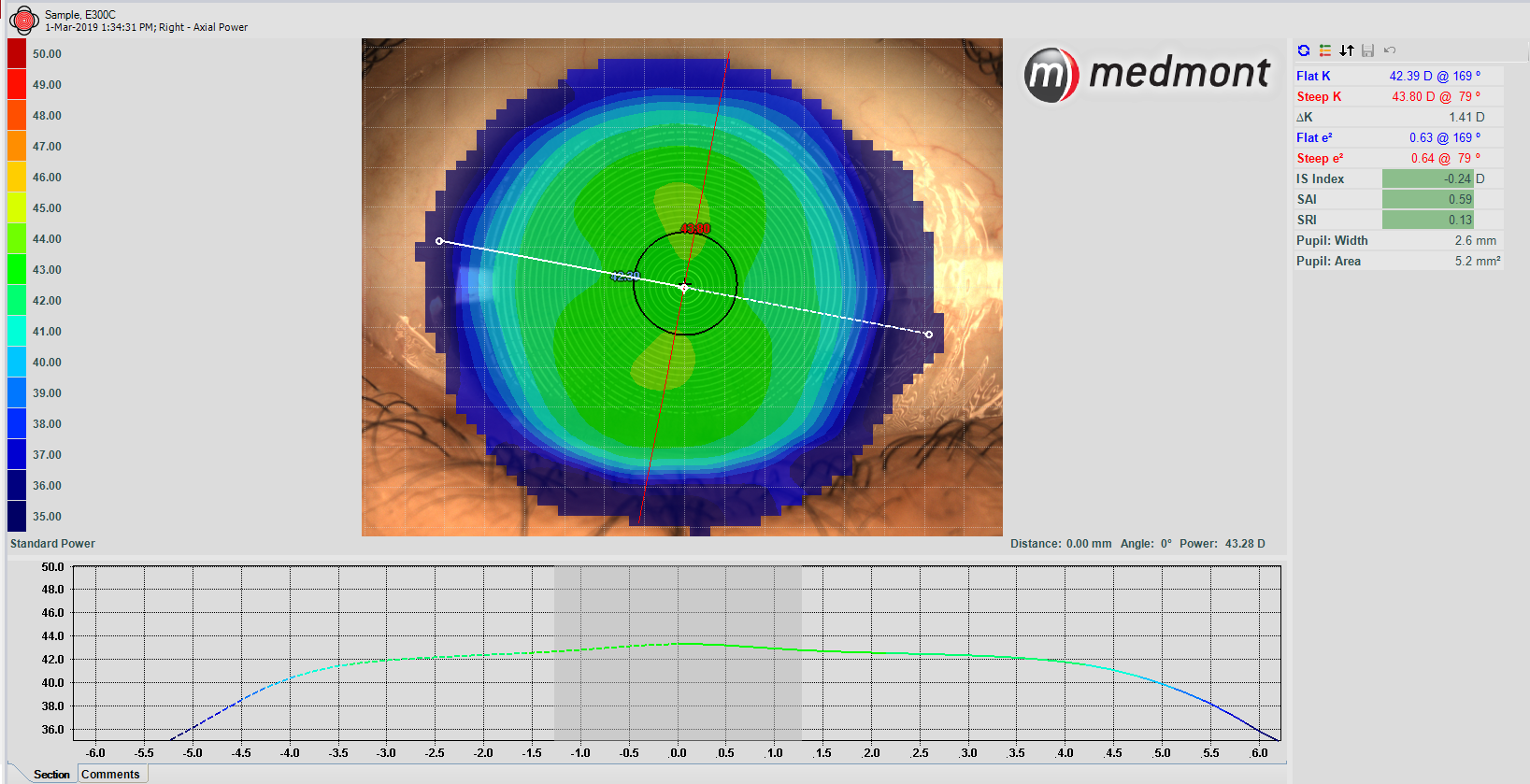
DED signs as seen through corneal topography include tear film instability and hyperosmolarity, which leads to increased ocular surface inflammation, damage, and neurosensory abnormalities. Even moderate DED can cause significant pain and limitations in performing daily activities. In severe cases, DED sufferers also may experience reduced energy, a decrease in general health, and even depression.
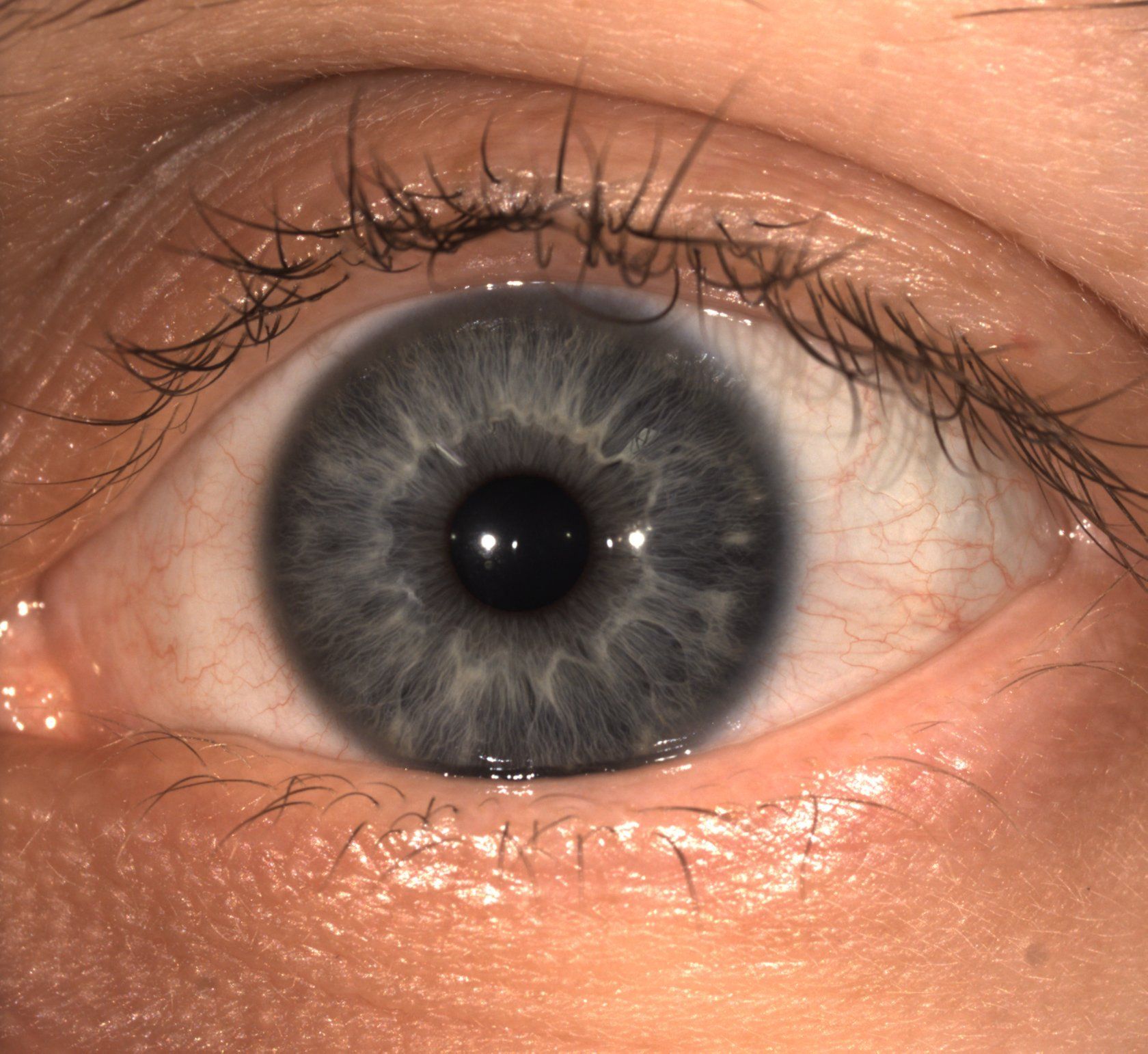
As optometry practices maximize time spent per patient and dig deeper into their health history, and conduct screenings for eye disorders such as DED, they help patients by focusing on maintaining their overall long-term health.
Anterior segment (AS) imaging devices with features such as corneal topography, AS photography, and meibography provide comprehensive DED diagnostics in a single, easy-to-use instrument.
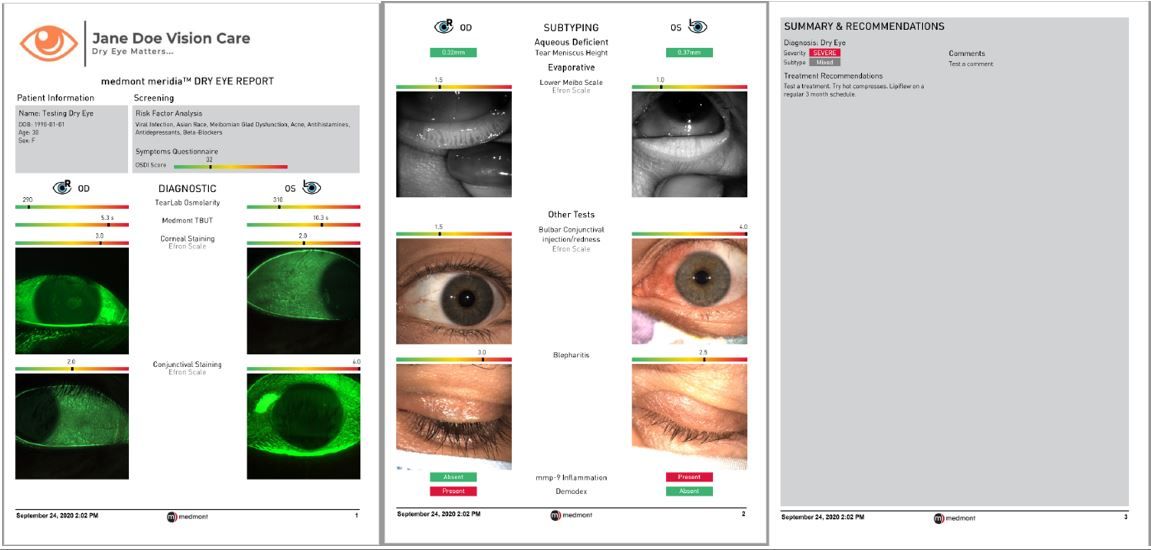
With easily digestible reports similar to optic nerve Optical coherence tomography, doctors provide meaningful and actionable diagnostic information while providing detailed ocular surface images that show patients the effects of DED. This is critical in helping patients understand their condition and promote treatment buy-in.
Doctor and patient engagement are the foundation of a positive patient experience. Thorough reporting through corneal topography enables patients to clearly understand the results of the DED screening, the suggested treatment plan, and see the progression in follow-up visits.
See the Future of DED Management at Optometry Practices
Practitioners can further utilize the increased time with patients to thoroughly educate their patients on DED, causes, treatment, and long-term management. Education on how to modify a patient’s environment, including increasing humidity, adjusting screen time when possible, as well as potential dietary modifications, are critical components of DED management. Ocular lubricants plus increased eyelid hygiene and warm compresses may also provide relief of symptoms.
For moderate to severe cases, practitioners can offer other treatments such as overnight topical ointments, in-office therapies, and longer-duration prescription steroids. This is not an exhaustive list of treatments; rather, it represents high-level options for rapid relief of symptoms post-diagnosis from a licensed practitioner. In conjunction with education, treatment, and management plan, the DED screening should be discussed, evaluated, and agreed upon between the practitioner and patient.
Healthy and happy eyes begin when you walk into your practitioner’s office. There is no one-size-fits-all treatment as every pair of eyes has particular needs and responds differently to treatment.
However, with proper education, tools, and corneal topography eye screening, DED can be successfully managed, preserving overall health and well-being. Regardless of treatment, the chronic nature of the condition often leads to reduced compliance over time. Continued monitoring with diagnostic testing is critical to track progression and effectiveness of treatment.
Open Your Patients’ Eyes
Are your patients some of the 50% of people living in the U.S. and Australia who don’t know about DED? Make screening for DED part of your routine check-ups and share this article on Facebook or LinkedIn to open other people’s eyes to dry eye disease.
